Human Papillomavirus
HPV-Associated Tumors
The risk for development of certain cancers is greater for people who have been infected with the human papillomavirus (HPV). As reported by the National Cancer Institute (NCI), HPV infection is responsible for an estimated 630,000 cancers worldwide each year, or approximately 5% of all cancers. 1Almost all cervical or throat (oropharyngeal) cancer is caused by HPV infection.
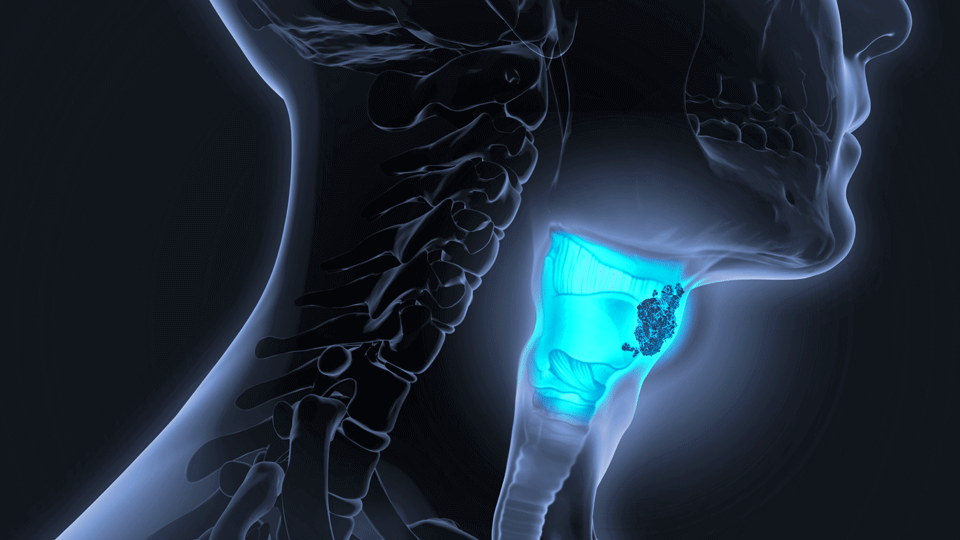
There are many types of HPV, and two of these, HPV 16 and HPV 18,2 are associated with the highest risk for development of cancers. HPV infection is common, and generally is propagated by sexual activity. While a person’s immune system may clear the infection, if it does not, and the infection persists for years, healthy cells may become cancerous.
Early vaccination against HPV is one way to prevent both HPV infection and the associated risk of cancer,3 but many people have not been vaccinated or the vaccine was not available before they become infected. This points to a need for treatment that reduces the risk of cancer, or may be able to treat HPV-associated cancer, in people already infected with HPV.
Human Papillomavirus (HPV) Clinical Trials
QUILT-3.100: Phase 1 Open-Label Study to Evaluate Safety And Determine The Maximum Tolerated Dose of IBRX-042 In Subjects With HPV-Associated Tumors.
We are conducting a phase 1 trial to study a vaccine, IBRX-042, targeting proteins produced by HPV after infection that has the potential to treat cancer in people infected with HPV. The vaccine uses a safe and effective method to deliver the vaccine proteins, called a human adenovirus serotype 5 (hAd5). The vaccine itself consists of two HPV proteins – E6 and E7. These proteins are safe to deliver on their own, will not cause HPV infection, and have been altered so that they cannot cause cancer. The have previously been shown to eliminate HPV4 in infected mice by stimulating the immune system to kill the virus.
The clinical trial will determine the maximum tolerable dose (MTD) of IBRX-042 in participants with HPV-associated cancer that have previously received treatment. Participants will be injected with IBRX under the skin (subcutaneously) 3 times (Day 1, 22, and 43). In the first participants in the study, the lowest dose will be tested, and in subsequent participants the dose will be increased if the lower dose is found to be safe. The response of each participant’s immune system to the vaccine will also be assessed. The highest dose of IBRX found to be both effective and safe may then be tested in a larger clinical trial to assess how effective it is in cancer treatment.
https://clinicaltrials.gov/ct2/show/NCT05976828
- The National Cancer Institute (NCI). HPV and Cancer. 2024. https://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-and-cancer
- Wolf J, et al. Human papillomavirus infection: Epidemiology, biology, host interactions, cancer development, prevention, and therapeutics. Rev Med Virol. 2024;34(3):e2537. https://onlinelibrary.wiley.com/doi/10.1002/rmv.2537
- Abbas K, et al.Yoo KJ. Equity impact of HPV vaccination on lifetime projections of cervical cancer burden among cohorts in 84 countries by global, regional, and income levels, 2010-2013: a modelling study. eClinicalMedicine. 2024; https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(24)00103-2/fulltext
- Wieking BG, Vermeer DW, Spanos WC, Lee KM, Vermeer P, Lee WT, et al. A non-oncogenic HPV 16 E6/E7 vaccine enhances treatment of HPV expressing tumors. Cancer Gene Ther. 2012;19(10):667-74. https://www.nature.com/articles/cgt201255.



